Analysis by Ashley Armstrong
Story at-a-glance
- Carbohydrates are essential for gut health. They protect your gut barrier by supporting the production of gastrointestinal mucus
- Adequate carbohydrate intake improves thyroid function, which enhances gut motility and helps prevent conditions like Small Intestinal Bacterial Overgrowth (SIBO)
- Whole food carbohydrates provide fiber that increases stool frequency and bulk, aiding in the elimination of toxins and maintaining gut health
- A balanced gut microbiome requires a low-oxygen environment, which is supported by the metabolism of carbohydrates and production of short-chain fatty acids
- Low-carb diets can provide short-term relief but may lead to reduced thyroid function and metabolic rate, negatively impacting digestive health in the long run
In recent years, carbohydrates have become the ultimate dietary scapegoat, blamed for everything from obesity to chronic disease. The rise of various low-carb diet trends has painted carbohydrates as the enemy of gut health and weight management, leading many to severely restrict or eliminate this essential macronutrient from their diets.
This villainization has been particularly prominent in both weight loss and gut health circles, where carbohydrates are often unfairly accused of being the primary culprit behind not only the obesity epidemic but also digestive disorders. A common misconception in gut health communities is that carbohydrates primarily “feed bad bacteria,” leading to dysbiosis and digestive issues.
However, this oversimplified view ignores the complex role carbohydrates play in human health, particularly in maintaining a healthy gut ecosystem. Scientific evidence consistently demonstrates their crucial role in maintaining gut health and overall digestive function. Understanding how carbohydrates support our gut health reveals why they’re not just beneficial, but essential for optimal wellness.
And of course when we say ‘carbs’ we are referring to whole food, real, single-ingredient carb sources like potatoes, rice, fruit, and quality-made bread. Processed, packaged ‘carbs’ contain a LOT more ingredients than just carbs … Plus, the calories that come from fat are often HIGHER than the calories that come from carbs for these foods.
For example — for a Krispy Kreme doughnut, the total calories are 190, total fat is 11 grams, total carbs is 22 grams, and total protein is 3 grams. 88 calories come from carbs, and 99 calories come from fat. So, is it really the “carbs”? Or do we need to separate and distinguish whole-food carbs and ultraprocessed foods?


Five Reasons Why Carbohydrates Improve Gut Health
1.Protect the gut barrier — One of the most crucial yet often overlooked benefits of carbohydrates is their role in protecting the gut endothelium. Glucose, the basic unit of carbohydrates, actively protects the gut endothelium against stress and helps maintains gut barrier integrity.1
This specialized tissue layer is fundamental to our health, controlling what passes between our bloodstream and gut tissue while supporting proper immune function and nutrient absorption. Proper function of the gut endothelium is essential for digestion and maintaining a balance in the gut microbiome.
2.Produce protective gastrointestinal mucous — Appropriate levels of mucus in the gut is vital for maintaining a healthy gut environment and supporting overall digestive health. Five important roles of mucus in the gut include:
•Protection — Mucus acts as a barrier that protects the intestinal lining from mechanical damage, pathogens, and toxins.
•Lubrication — It helps facilitate the passage of food and waste through the digestive tract, making digestion and excretion smoother.
•Immune function — Mucus contains antibodies and antimicrobial proteins that help defend against infections by neutralizing harmful bacteria and viruses.
•Microbiome support — It provides a habitat for beneficial gut bacteria, which are essential for digestion, nutrient absorption, and overall gut health.
•Hydration — Mucus helps maintain moisture in the gut, which is important for proper digestive function.
Well, carbs (and protein!) are the building block of this important mucus layer.
“The major building blocks in mucus are mucins, which are large, highly glycosylated proteins. Typically, these mucins are >80% carbohydrate, and are concentrated into mucin domains.”2
Glycosylated proteins are proteins that have sugar molecules (glycans) attached to them.
3.Speed up transit time — A lesser-known but significant aspect of carbohydrate consumption is its positive impact on thyroid health, which directly influences digestive function. Research consistently shows that carbohydrate consumption improves thyroid health,3 and better thyroid health leads to faster gastric emptying times.4,5
Proper gut motility and a relatively fast emptying time is crucial for preventing conditions like Small Intestinal Bacterial Overgrowth (SIBO). Poor gut motility leads to stagnation, which then results in bacterial overgrowth and fermentation in the wrong spots along the digestive tract, leading to pain, bloating, food intolerances and other digestive issues.
Thyroid hormones play a crucial role in gut motility by modulating the enteric nervous system, altering smooth muscle function, and regulating the Migrating Motor Complex (MMC).6,7 The MMC is a series of muscle contractions that occur in our gut during fasting periods between meals. The primary function of the MMC is to clean up the digestive tract after we’ve finished processing a meal.
Just as we clean the kitchen after cooking, our body needs to “clean up shop” before the next meal. This process is crucial for maintaining a healthy digestive environment.
Understanding the relationship between energy production and gut health is crucial. As Dr. Ray Peat noted, “Energy and structure are interdependent, at every level.” Proper function requires adequate structure, and adequate structure requires sufficient energy. So, proper functioning of the digestive tract relies on adequate systemic energy production.
4.Increases poop frequency and bulk — Pooping every single day is a must! Poop isn’t just food waste; it contains a variety of other components, including:
•Bacteria — A significant portion of stool is made up of bacteria, both living and dead, which play a role in digestion and overall gut health.
•Cellular debris — This includes dead cells from the intestinal lining and immune cells.
•Toxins — The body eliminates certain toxins and waste products through the intestines, including substances that may have been processed by the liver.
•Used hormones — Hormones that are no longer needed or have been metabolized can also be excreted in feces.
•Bile salts — Bile, produced by the liver and stored in the gallbladder, aids in fat digestion and is excreted in stool, giving it its characteristic color.
So, your poop is a complex mixture of materials that the body needs to eliminate to maintain homeostasis and health.
Without pooping every day, 90% to 95% of bile, which contains toxins, mycotoxins, pesticides, xenobiotics and excess hormones can be recirculated in your body through a process called enterohepatic recirculation.
When consuming whole food carbohydrate sources such as potatoes, fruits, starches, and sourdough bread, you aren’t just boosting thyroid health, but you’re also getting beneficial fiber. Both soluble and insoluble fiber play crucial roles in gut health. Soluble fiber binds to bile acids, helps eliminate used hormones, and assists in removing fat-soluble toxins.
Insoluble fiber adds bulk to stool, supports regular bowel movements, and helps maintain gut transit time.
You don’t have to go out of your way to go cray overboard in consuming fiber, but moderate amounts through the consumption of whole foods is well documented in the literature to support and improve overall gut health.8,9,10
5.Keep the microbiome balanced, naturally — While it is near impossible to define what the ideal microbiome should look like (resident microbes are highly diverse, vary between individuals, and change with diet), recent evidence supports that the ideal gut microbiome should be dominated by obligate anaerobic bacteria that can break down nonusable fibers, with lower levels of facultative organisms.11
Obligate anaerobic bacteria specialize in fiber consumption and help maintain the right internal conditions to support healthy gut bacteria. Facultative anaerobic bacteria, on the other hand, may interfere with host nutrition and produce problematic endotoxins.
Now, we will always have some amount of both obligate and facultative species, but balanced gut microbiomes are characterized by the dominance of obligate organisms, while an expansion of facultative organisms is a common marker of gut dysbiosis.
We want more obligate anaerobic bacteria, but these beneficial species cannot survive in high oxygen environments. (While facultative anaerobes, on the other hand, grow well in the presence of oxygen.) So, maintaining a LOW oxygen environment and thus a HIGH CO2 environment in our gut helps keep the microbiome in check.
And how do we maintain a low oxygen environment? The metabolism of the cells that line your gut, meaning how they make energy, changes the internal environment of the gut, thus impacting the types of bacteria that can thrive.
These cells have two options for energy production: beta oxidation or glycolysis. Ideally, they perform oxidative phosphorylation through beta oxidation of short chain fatty acids (SCFAs) — that can come from our diet but are largely produced from obligate anaerobes breaking down fiber in our gut.
The oxidation of SCFAs consumes high amounts of oxygen, which then maintains a low oxygen environment inside the colon. So, it is important to maintain high levels of SCFAs in the gut!
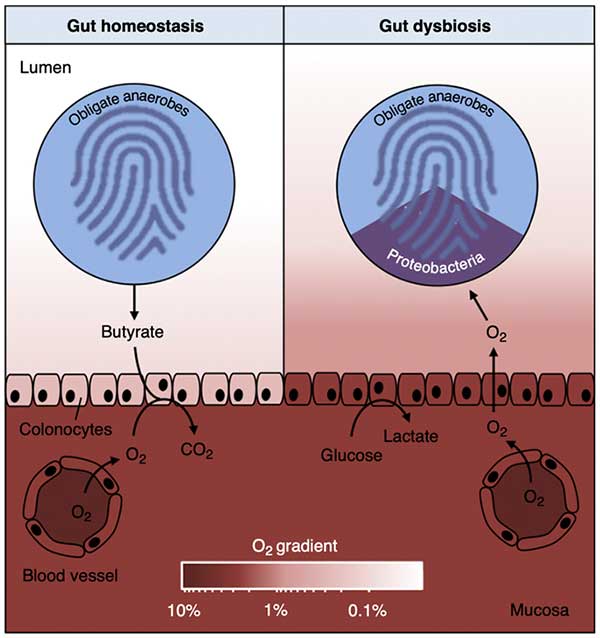 During gut homeostasis (left), b-oxidation of microbiota-derived butyrate causes epithelial hypoxia, which maintains anaerobiosis in the lumen of the large bowel. In turn, luminal anaerobiosis drives a dominance of obligate anaerobic bacteria within the gut microbiota. During gut dysbiosis (right), surface colonocytes obtain energy by anaerobic glycolysis, which leads to increased epithelial oxygenation. This epithelial dysfunction disrupts anaerobiosis in the lumen, thereby driving an expansion of facultative anaerobic Proteobacteria by aerobic respiration. The color scale shown at the bottom (O2 gradient) indicates oxygen availability. Image from: COMICR Volume 39, October 2017, Pages 1-6.
During gut homeostasis (left), b-oxidation of microbiota-derived butyrate causes epithelial hypoxia, which maintains anaerobiosis in the lumen of the large bowel. In turn, luminal anaerobiosis drives a dominance of obligate anaerobic bacteria within the gut microbiota. During gut dysbiosis (right), surface colonocytes obtain energy by anaerobic glycolysis, which leads to increased epithelial oxygenation. This epithelial dysfunction disrupts anaerobiosis in the lumen, thereby driving an expansion of facultative anaerobic Proteobacteria by aerobic respiration. The color scale shown at the bottom (O2 gradient) indicates oxygen availability. Image from: COMICR Volume 39, October 2017, Pages 1-6.Recent research has revealed that lowering dietary carbohydrate intake can decrease the concentration of SCFAs and SCFA producing bacteria.12 Low-carb, high-protein diets have also been shown to foster a pathogenic and proinflammatory microbiota profile, increase ammonia, phenol, and hydrogen sulfide production, and drive mucosal inflammation and other intestinal issues.13
While low-carb diets can provide short-term relief, in the long-term cutting carbs is a band-aid approach to avoid dealing with a slow metabolism. It’s not fixing the underlying metabolic problem and low energy state that led to the gut problems to begin with.
Low-carb diets increase stress hormones and there is an abundance of research showing that low-carb diets result in reduced active thyroid hormone T3,14 increase thyroid blocking hormone rT3, and reduce metabolic rate and energy production — all of which will negatively impact digestive health in the long run.15
Avoid Restrictive Extremes
The common ‘starving’ approach to gut problems may provide temporary relief but the condition will return because you didn’t address the initial reason why the imbalance occurred — low metabolic rate.
Plus, you can NEVER win the war against bacteria by trying to starve it. Bacteria multiply by 2 every 12 hours. So, if you starve the bacteria, the stuff that grows back will be all replicas of the bacteria that is immune to starvation. This is evolution at its finest and nature will always win.
Rather than taking extreme measures or attempting to micromanage the gut microbiome, a more balanced, holistic approach is recommended:
- Focus on improving overall metabolic rate and systemic function, which involves including dietary carbs, that will address intestinal motility
- Remove gut-irritating foods for your unique gut
- Temporarily eliminate individual trigger foods
- Provide adequate energy and nutrients
- Allow the body’s natural healing mechanisms to work
So, what carbs work best for you? The goal here is to identify foods that can be more fully digested and thus minimize digestive discomfort. Not all carbs will work for everyone! If certain foods don’t agree with you right now (which can totally change as gut health and thyroid health improves), avoid them for the time being.
Try to select foods that you objectively do well with, but we don’t want to be super restrictive with carbs or overall calorie intake as this can negatively impact thyroid health.

Save This Article for Later – Get the PDF Now
The Good News: Gut Health Is Highly Adaptable
One of the most encouraging aspects of gut health is its ability to regenerate and adapt quickly! The gut lining is replaced every three days16 and the gut microbiome can change within a single day based on dietary choices.17
When increasing carbohydrate intake, it’s important to start slowly and focus on whole food sources. Pay attention to your individual response to avoid digestive discomfort and try to maintain consistent as you reintroduce. Best sources of gut-friendly carbohydrates:
- Rice
- Sourdough bread, or quality made bread using well-sourced grains
- Root vegetables like potatoes and sweet potatoes (if you can find Japanese sweet potatoes or purple sweet potatoes, they taste so much better than the orange variety!)
- Fresh, ripe fruits
- Masa harina, or traditionally made tortillas
Some people also do well with soaked and well-cooked legumes. Not all carb sources will work for everyone! Individual responses to different types of carbohydrates can vary significantly, as the state of our own microbiome will determine the effect different types of fibers have on us. So, it is important to focus on the carb sources that work well for you!
Signs of Healthy Gut Function
Indicators of good gut health (and what we are shooting for) include:
- Regular bowel movements (1 to 3 times daily)
- Minimal bloating or discomfort
- The ability to digest a wide variety of food
- Good energy levels
- Proper nutrient absorption
With a well-functioning metabolism, the above IS possible!
Conclusion
Carbohydrates play a vital role in maintaining gut health through multiple mechanisms. From protecting the gut barrier and supporting thyroid function to feeding beneficial bacteria and maintaining proper motility, carbohydrates are essential for optimal digestive function.
The key lies in choosing the right types of carbohydrates that work for you and understanding that gut health is part of a larger systemic picture involving energy production and metabolism. By taking a balanced, informed approach to carbohydrate consumption, we can support our gut health while avoiding the pitfalls of extreme dietary restrictions and food fear.
Remember that the goal isn’t to manipulate the microbiome directly but to provide the body with the tools and resources it needs to maintain optimal gut health naturally. When we support our body’s natural processes through proper nutrition, including adequate carbohydrate intake, we give the body the tools it needs to create the conditions for optimal gut health and overall well-being.
Transform Your Health — One Step at a Time

Ashley and her sister Sarah have put together a truly groundbreaking step-by-step course called “Rooted in Resilience.” They have compiled what clearly is the best application of Dr. Ray Peat’s work on Bioenergetic Medicine that I have ever seen.
It is so good that I am using the core of their program to teach the many Health Coaches that I am in the process of training for the new Mercola Health Clinics I am opening this fall. It took these women working nearly full-time on this project for a year to create it.
This has to be one of the absolute best values for health education I have ever seen. If you want to understand why you struggle with health problems and then have a clear program on how to reverse those challenges, then this is the course for you.
It is precisely the type of program I wish I would have had access to when I got out of medical school. I fumbled around for decades before I reached the conclusion they discuss in the course and share with you so you can restore your cellular energy production and recover your health.
| Select and eat the right foods to heal your metabolism and improve glucose utilization |
| Balance your hormones to help reduce anxiety, weight gain and sleep disturbances |
| Use reverse dieting to increase your calories without gaining weight and tanking your metabolism, all while improving your energy levels |
| Heal your gut for proper immune function, mood and weight management |
| Tweak your diet and lifestyle habits to improve your mindset and mental health |
| Crush your fitness goals with ease and get your life back on track |
| Master the most essential habits for health with bonus guides, including over 100 meal plans to take the stress out of meal time planning and shopping, and so much more! |
Learn more about Rooted in Resilience here.

About the Author
Ashley Armstrong is the co-founder of Angel Acres Egg Co., which specializes in low-PUFA (polyunsaturated fat) eggs that are shipped to all 50 states (join waitlist here), and Nourish Cooperative, which ships low-PUFA pork, beef, cheese, A2 dairy and traditional sourdough to all 50 states. Waitlists will reopen shortly.
- 1 Histol Histopathol. 2017 Jun;32(6):543-550. doi: 10.14670/HH-11-839. Epub 2016 Nov 8
- 2 Nat Rev Gastroenterol Hepatol. 2013 Mar 12;10(6):352–361
- 3 Indian J Endocrinol Metab. 2014 May-Jun; 18(3): 307–309
- 4 Gastroenterol Res Pract. 2010 Mar 7;2009:529802
- 5 Isr J Med Sci. 1997 Mar;33(3):198-203
- 6 Neuropeptides. 1996 Jun;30(3):237-47. doi: 10.1016/s0143-4179(96)90070-0
- 7 Handbook of Clinical Neurology 86:343-55, DOI: 10.1016/S0072-9752(07)86017-9
- 8 Am J Clin Nutr. 2018 Mar 1;107(3):436-444. doi: 10.1093/ajcn/nqx082
- 9 Nutr Neurosci. 2023 Feb;26(2):108-126. doi: 10.1080/1028415X.2021.2020403. Epub 2022 Jan 4
- 10 Am J Epidemiol. 2014 Sep 15;180(6):565-73. doi: 10.1093/aje/kwu174. Epub 2014 Aug 20
- 11 Science. 2018 Nov 30; 362(6418): eaat9076
- 12 Appl Environ Microbiol. 2006 Dec 22;73(4):1073–1078
- 13 Aliment Pharmacol Ther. 2016 Jan;43(2):181-96. doi: 10.1111/apt.13456. Epub 2015 Nov 2
- 14 J Am Coll Nutr. 1985;4(4):451-9. doi: 10.1080/07315724.1985.10720087
- 15 Diabete Metab. 1982 Dec;8(4):299-305
- 16 Front. Cell Dev. Biol., 12 November 2020 Sec. Stem Cell Research Volume 8 – 2020
- 17 Sci Transl Med. 2009 Nov 11;1(6):6ra14. doi: 10.1126/scitranslmed.3000322


















Thanks! Share it with your friends!
Tweet
Share
Pin It
LinkedIn
Google+
Reddit
Tumblr