Analysis by Dr. Joseph Mercola
STORY AT-A-GLANCE
- An analysis of medical records revealed a direct correlation between levels of vitamin D and the severity of illness in people infected with SARS-CoV-2
- Low vitamin D levels are normally found in people with dark skin. This may be a compelling factor in the higher rates of COVID-19 illness and mortality
- The U.K. recommends vitamin D supplementation during this pandemic, concerned people are not getting enough sunlight; yet the U.S. continues to focus on drugs and vaccine production
- Vitamin D needs vary widely, so it’s important to get your levels tested before deciding how much vitamin D3 supplement you should take
There is strong scientific evidence vitamin D plays a central role in your immune response and your ability to fight infections. In this video, Ivor Cummins, biochemist and chief program officer for Irish Heart Disease Awareness, explains how recent studies supporting higher levels of vitamin D may reduce your risk of negative outcomes from COVID-19.
He also singles out some of the conditions associated with low vitamin D levels, such as low sun exposure, insulin resistance and high levels of inflammation.
In 2017, a review of randomized, double-blind, placebo-controlled trials using vitamin D2 or D3 was published in the BMJ.1 The data revealed vitamin D supplementation was “safe and it protected against acute respiratory tract infection overall.” They found people who were most deficient experienced the greatest benefit.
I am beyond excited to announce a groundbreaking new study by an organization that we have supported for over 15 years, GrassRootsHealth. Many of you have ordered their vitamin D test in the past, and the funds from that were used to do this clinical trial that could change the entire treatment strategy for COVID-19.
A recent clinical trial to investigate the efficacy of vitamin D against COVID-19 was announced April 3, 2020.2 Days later, Mark Alipio — who received no funding for his work — published a preprint letter3 in which he released data from an analysis of 212 people with lab-confirmed COVID-19 and for whom there were serum 25(OH)D levels available. You can read Alipio’s full study here.
Using a classification of symptoms based on previous research, he employed statistical analysis to compare the differences in clinical outcomes against the levels of vitamin D. Of the 212 people, 49 had mild disease; 59 had ordinary disease; 56 were severe and 48 were critical.
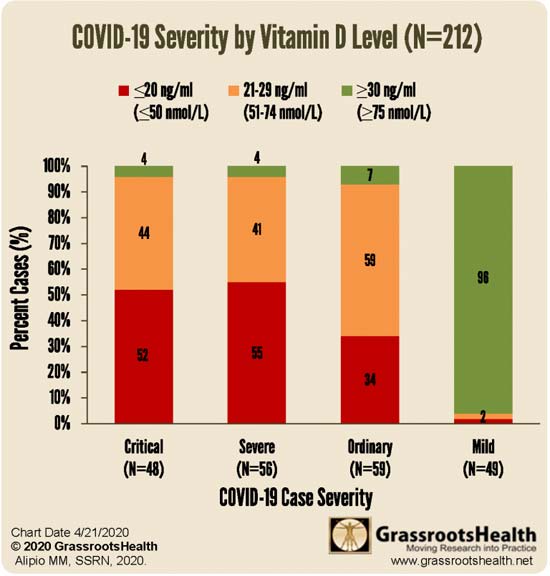
In the initial study group of 212 patients (see Table 1 below), 55 had normal vitamin D levels, which Alipio defined as greater than 30 ng/ml; 80 had insufficient levels of 21 to 29 ng/ml and 77 had deficient levels of less than 20 ng/ml. Vitamin D levels were strongly correlated to the severity of the illness experienced. It is important to note that most experts consider 30 ng/ml half of what an optimum vitamin D level should be, which is 60 to 80 ng/ml.
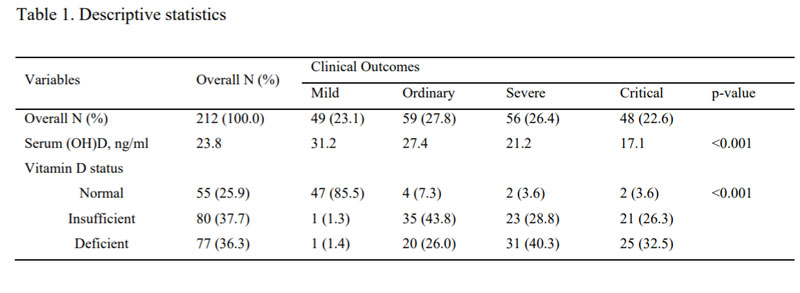
Of the 49 with mild illness, 47 had normal vitamin D levels. For those of you who are not good with math that means that 96% of the patients with mild illness had “normal” levels of vitamin D. Note again this “normal” level was above 30, and most experts would raise that to 60.
Of the combined 104 with severe or critical illness, only four had normal levels of vitamin D. That is 4% or the reciprocal of the mild group. How much stronger a correlation could one hope for? Alipio concluded:4
“… this study provides substantial information to clinicians and health policy-makers. Vitamin D supplementation could possibly improve clinical outcomes of patients infected with Covid-2019 based on increasing odds ratio of having a mild outcome when serum (OH)D level increases. Further research may conduct randomized controlled trials and large population studies to evaluate this recommendation.”
Further Evidence Vitamin D Significantly Impacts Outcomes
The writers of a recent editorial in Alimentary Pharmacology & Therapeutics5 used a different metric, but arrived at similar results. They argued a marked variation in mortality occurs above or below 35 degrees North latitude. This is also the line above which it is not possible for people to get enough sunlight to retain vitamin D during the winter months.
When the mortality per million is plotted against latitude, the results suggest vitamin D plays a role in the outcome of infection with SARS-CoV-2. Data were gathered from countries reporting more than 150 people infected by April 15, 2020.
Although Nordic countries are far north of the demarcation line, vitamin D deficiency is also relatively low, potentially from widespread use of supplements. In countries where deficiency is common, such as Spain and Italy, mortality rates have been higher. The writers stress the importance of vitamin D on the outcome of infection, concluding that, while there is modest evidence, it protects against infection:6
“… the hypothesis is not that vitamin D would protect against SARS-CoV-2 infection but that it could be very important in preventing the cytokine storm and subsequent acute respiratory distress syndrome that is commonly the cause of mortality.”
A second paper7 published in April 2020 hypothesized that vitamin D protects the body against SARS-CoV-2 infections and sought to assess if there was an association between vitamin D levels and the number of COVID-19 infections. The data included only European countries and found a significant relationship between the mean (average) vitamin D level and the number of infections.8
People who were most vulnerable to this respiratory infection were the most deficient. They concluded the results support the advice to supplement with vitamin D to protect against the SARS-CoV-2 infection. These results support the 2017 review of studies published in the BMJ noted above.9
Yet another paper evaluated the role vitamin D deficiency plays in preventing respiratory infections and found similar results.10 The researchers wrote that vitamin D had “a significant protective effect” and reduced the risk of an acute respiratory infection from 60% to 32% in participants. The researchers also wrote vitamin D may help prevent respiratory infections and lower antibiotic use.
African-Americans Experiencing Higher Rates of Infection
A letter to the editor was then published in the BMJ, signed by 30 scientists from around the world, including Alipio.11 They pointed out the disproportionately high number of individuals who are Black, Asian and Minority Ethnic (BAME), or those living in care homes in the U.K. who die from COVID-19.
They also identified obesity as another risk factor, with co-morbid conditions including diabetes and cardiovascular disease. Each group of people — those living in care homes, BAME and obese — also tends to have lower levels of vitamin D.
The letter included the research results from Alipio’s preprint letter, indicating the 30 scientists agreed with how the data was collected and analyzed, as well as the conclusions. The group identified the lengthy process vaccines require and the 100 years of research on vitamin D.
They hypothesized that vitamin D has clinical relevance to COVID-19 and may reduce the number of fatalities. Although there is a need for clear clinical evidence with research, it’s important to note the widespread vitamin D deficiency, including the risk groups mentioned. They quote Dr. Hugh Sinclair, who nearly 100 years ago observed:12
“The deficiency of any nutrient which is essential for every tissue will eventually lead to abnormal function in every tissue. That is so incontrovertibly obvious that I am continually astonished it must be repeatedly forcefully restated.”
They then went on to give a reason for why vitamins have so often been overlooked:13
“Human nature is such that simple solutions to complex issues, for example vitamin C for scurvy, and hand washing prior to baby delivery, are often not readily embraced; but surely the scale and impact of the COVID-19 pandemic demands all avenues are fully explored; more so when no other effective treatment strategies as yet exist.
A safe simple step, the correction of a deficiency state, vitamin D this time, convincingly holds out a potential, significant, feasible ‘COVID-19 mitigation remedy.”
Others connect the heavy toll in the African-American community with an increased prevalence of obesity, diabetes and high blood pressure, which are risk factors for increased severity of COVID-19.14 In the states of Maryland and Louisiana and the metropolises of New York, Chicago and Washington, D.C., the percentages of BAME individuals dying from probable COVID-19 are higher than the percentages of BAME who live in the area.
However, while there is a correlation between the higher prevalence of health conditions that increase disease severity in the African-American population, there is also a higher prevalence of vitamin D insufficiency due to reduced production.15 Darker pigmentation produces less vitamin D with exposure to the sun.
Vitamin D in COVID-19 Treatment
Findings from The Irish Longitudinal Study on Ageing (TILDA)16 and a vitamin D review paper17 published in the journal Nutrients, April 2, 2020, also suggest vitamin D deficiency could have serious implications for COVID-19. As reported by Medical Xpress, April 6, 2020:18
“The report,19 ‘Vitamin D deficiency in Ireland — Implications for COVID-19. Results from the Irish Longitudinal Study on Ageing (TILDA),’ finds that vitamin D plays a critical role in preventing respiratory infections, reducing antibiotic use, and boosting the immune system response to infections.
With one in eight Irish adults under 50 deficient in vitamin D, the report highlights the importance of increasing intake … TILDA researchers recommend that adults over 50 should take supplements — not just in winter, but all year round if they don’t get enough sun …
Professor Rose Anne Kenny, principal investigator of TILDA, said: ‘We have evidence to support a role for vitamin D in the prevention of chest infections, particularly in older adults who have low levels. In one study Vitamin D reduced the risk of chest infections to half in people who took supplements.
Though we do not know specifically of the role of vitamin D in COVID infections, given its wider implications for improving immune responses … at-risk cohorts should ensure they have an adequate intake of vitamin D.'”
The second paper, published in the journal Nutrients, carries the telling title, “Evidence That Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Death.”20 As reported in the abstract:
“This article reviews the roles of vitamin D in reducing the risk of respiratory tract infections, knowledge about the epidemiology of influenza and COVID-19, and how vitamin D supplementation might be a useful measure to reduce risk. Through several mechanisms, vitamin D can reduce risk of infections.
Those mechanisms include inducing cathelicidins and defensins that can lower viral replication rates and reducing concentrations of pro-inflammatory cytokines that produce the inflammation that injures the lining of the lungs, leading to pneumonia, as well as increasing concentrations of anti-inflammatory cytokines …
Evidence supporting the role of vitamin D in reducing risk of COVID-19 includes that the outbreak occurred in winter, a time when 25-hydroxyvitamin D (25(OH)D) concentrations are lowest; that the number of cases in the Southern Hemisphere near the end of summer are low …
Vitamin D deficiency has been found to contribute to acute respiratory distress syndrome; and … case-fatality rates increase with age and with chronic disease comorbidity, both of which are associated with lower 25(OH)D concentration.
To reduce the risk of infection, it is recommended that people at risk of influenza and/or COVID-19 consider taking 10,000 IU/d of vitamin D3 for a few weeks to rapidly raise 25(OH)D concentrations, followed by 5000 IU/d. The goal should be to raise 25(OH)D concentrations above 40–60 ng/mL (100–150 nmol/L). For treatment of people who become infected with COVID-19, higher vitamin D3 doses might be useful.”
UK Recommends Supplementation
Public Health England is recommending their citizens take a vitamin D supplement while they are spending more time indoors.21 The National Health Service22 routinely recommends their citizens take a supplement during the fall and winter months. They also recommend a supplement all year round for those who aren’t outdoors, are in a care home, usually cover all their skin or have dark skin.
The chief nutritionist at Public Health England is concerned that Britons may not be getting enough vitamin D from sunlight as they spend more time indoors. They counsel their citizens that while an adequate amount of vitamin D cannot stop an infection, it does have benefits, including improved outcomes in those who are deficient.23
Yet, despite radical changes in the way people are living during the pandemic, the guidelines in the U.S. have not changed. The National Institutes of Health recommends that most people get their nutrients from food and beverages, including fortified food products. However, dietary intake is not sufficient to maintain healthy levels:24
“Dietary intake of vitamin D from natural foods traditionally plays only a minor role with few available natural sources: animal sources such as fatty fish, cod liver oil, or egg yolks contain vitamin D3, and fungal sources such as mushrooms and yeast exposed to sunlight or UV radiation contain vitamin D2 (ergocalciferol).”
The U.S. health agencies appear to have little interest in helping the public support their immune system through appropriate nutrition but would rather rely on drugs and vaccines.
Some Public Health Officials Recognize Value of Vitamin D
Although the official recommendation from government agencies is to wait for drugs and a vaccine, some are speaking out. Former CDC director Dr. Tom Frieden wrote an opinion piece for Fox News in which he suggests vitamin D may reduce COVID-19 mortality rates, especially in those who are deficient.25
He goes on to say supplementation has reduced the “risk of respiratory infections, regulates cytokine production and can limit the risk of other viruses such as influenza.” Much of the damage from COVID-19 occurs with a “cytokine storm,” during which the body’s inflammatory system goes into high gear, damaging organs and increasing mortality rates.
The evidence of seasonality of some viral infections may be related to vitamin D production that declines during the winter months. Seasonal changes in infection rates are more evident in northern climates, and little or none in areas that are warm all year. He concluded:26
“We can do lots of things to improve our resistance to infection. These include getting regular physical activity, getting enough sleep, stopping smoking and other tobacco use, and, for people living with diabetes, getting it under control. Taking a multivitamin that includes Vitamin D, or a Vitamin D supplement, probably can’t hurt, and it might help.
As we continue to work to mitigate the impact of COVID-19, anything we can do to strengthen our resistance is a step in the right direction.”
Dr. John C. Umhau was a public health specialist at the National Institutes of Health for over 20 years. In an article in MedPageToday he referenced his review in which he argued there were groups who were more likely to have vitamin D deficiency, including those who are obese, the elderly and those with dark skin. Yet vitamin D is one of the:27
“… most studied and most important host factor impacting survival from COVID-19 … A government-sponsored research strategy to address this issue has not been developed, as officials explained that there was no mandate to explore an alternative to the existing vaccination program.
However, other researchers picked up the ball and provided convincing evidence that vitamin D could reduce the incidence of acute respiratory infection.”
In further evidence published in Nutrients,28 scientists reviewed how vitamin D can reduce the risk of infection by lowering the rate at which the virus replicates and reduce the pro-inflammatory cytokines that damage the lungs, leading to pneumonia. Vitamin D also helps increase concentrations of anti-inflammatory cytokines that may help protect the lungs. The researchers recommended those at risk take:
“… 10,000 IU/d of vitamin D3 for a few weeks to rapidly raise 25(OH)D concentrations, followed by 5000 IU/d. The goal should be to raise 25(OH)D concentrations above 40–60 ng/mL (100–150 nmol/L).”
Individuals Dosages Vary Widely — Test To Be Sure
Although the researchers recommended a specific amount of vitamin D3 to take, it’s impossible to predict how much supplementation you personally may need unless your blood level is measured. Typically, ranges are from 2,000 to 10,000 units (IUs) per day, but there are many variables that contribute to this dose — that is why testing is so important.
By testing at home you can stay away from hospitals unless you’re having symptoms of a worsening respiratory infection, such as difficulty breathing. Ideally, you’d like your level to be 60 ng/mL.
GrassrootsHealth makes testing easy by offering an inexpensive vitamin D testing kit as part of its consumer-sponsored research. All revenues from these kits go directly to GrassrootsHealth. I make no profit from these kits and only provide them as a service of convenience to my readers.
For more information about supporting your immune system, fighting the SARS-CoV-2 virus and additional nutraceuticals that have demonstrated a positive effect on your immune system or fighting viral infections, see “Quercetin and Vitamin D — Allies Against Coronavirus?”
Interesting Note on Fauci and Vitamin D
As reviewed in an earlier article, long before SARS-CoV-2 became part of everyday life, Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases (NIAID), believed vitamin C and D were important strategies for enhancing your body’s immune system. Just four years ago, he was interviewed by a reporter from Washingtonian on how to avoid getting sick.
He explained the importance of washing your hands, clipping your nails and getting enough sleep. A fourth strategy he discussed was using vitamin C and D supplements:29
“It can enhance your body’s defense against microbes. I take 1,000 milligrams a day. Many people also do not get enough vitamin D, which affects a lot of body functions, so that would be helpful, too.”
In the current pandemic, the U.S. has placed inexpensive, patent-free nutritional supplements in second place to drugs and vaccines, which come with a high price tag in addition to unwelcome side effects.
In a more recent interview with RealClearPolitics, Fauci appeared to hedge his opinion. He stressed the viability of vitamin C as an antioxidant that’s “essentially totally harmless unless you take in a ridiculous amount.”
But when asked whether vitamin D might mitigate some respiratory infections, he said: there’s “no definitive proof.” He did point out, though, that you’re not likely to get hurt by it.30 Still, his answers suggest an unwillingness to admit vitamin D plays a proven and important role in infectious disease.
Might Fauci’s backpedaling on vitamins C and D have anything to do with the fact that he serves on the Leadership Council for the Bill & Melinda Gates Foundation’s Global Vaccine Action Plan? He describes his litmus test for safety and effectiveness as being tied to randomized control trials:31
“That’s why you keep hearing me over and over again saying the best optimal way is to do a randomized control trial to determine as quickly as possible whether something works, and if it does, get it out there. If it doesn’t, get it off the table.”
In what appears contradictory to this statement, Fauci said a vaccine may be released in the next 12 to 18 months.32 However, the standard steps to develop a relatively “safe” vaccine averages five years. It begins with two to four years of laboratory research, followed by one to two years of preclinical studies, and then Phase I, II and III trials.33
- 1, 9 the BMJ, 2017;356:j6583
- 2 Clinical Trials, April 3, 2020
- 3, 4 Grassroots, April 9, 2020
- 5, 6 Alimentary Pharmacology & Therapeutics, 2020; doi.org/10.1111/apt.15777
- 7 Europe PMC, 2020; DOI: 10.21203/rs.3.rs-21211/v1 Abstract
- 8 NY Post, May 1, 2020
- 10 The Irish Longitudinal Study on Aging, April 2020; doi.org/10.380108/TildaRe.2020-05
- 11, 12, 13 the BMJ, April 24, 2020
- 14 CBS News, April 23, 2020
- 15 Journal of Nutrition, 2006;136(4)
- 16, 19 TILDA.tcd.ie Vitamin D deficiency in Ireland — Implications for COVID-19. Results from the Irish Longitudinal Study on Ageing (TILDA)
- 17, 20 Nutrients April 2, 2020; 12(4): 988
- 18 Medical Xpress April 6, 2020
- 21 CNN, April 23, 2020
- 22 National Health Service
- 23 BBC, April 23, 2020
- 24 Frontiers in Endocrinology, 2018;9:373
- 25, 26 Fox News, March 23, 2020
- 27 MedPageToday, March 25, 2020
- 28 Nutrients, 2020;12:988 Abstract; last line
- 29 Washingtonian, January 15, 2016
- 30, 31 RealClear Politics, March 26, 2020
- 32 Business Insider, April 1, 2020
- 33 The History of Vaccines
















Thanks! Share it with your friends!
Tweet
Share
Pin It
LinkedIn
Google+
Reddit
Tumblr