Analysis by A Midwestern Doctor
STORY AT-A-GLANCE
- One of aging’s most profound consequences is the gradual weakening of bones, which can lead to life-altering physical limitations and fractures. Currently, we wisely aim to prevent bone loss early on but unwisely rely on routine bone density scans, often leading to the indiscriminate sale of “bone-strengthening” drugs to a large patient base
- This approach is deeply flawed. Scan data frequently fails to reflect true bone strength, while increasing density often results in brittle bones prone to fracture. Moreover, the commonly prescribed bone density drugs carry significant risks
- In the face of a lucrative drug market (such as osteoporosis affecting 20% of women over 50), the medical industry dismisses alternative approaches that do not generate substantial profits
- This profit-driven mindset leaves us with little understanding of osteoporosis’s true causes or the most effective treatments. This article will delve into the forgotten knowledge of bone health
The years I have spent studying the medical industry have made me appreciate how often economic principles can allow one to understand its complex and contradictory behavior.
For example, I believe many of the inconsistencies in medical ethics (e.g., “mothers have an absolute right to abort their children” and “mothers cannot refuse to vaccinate their children because it endangers their child’s life”) can be explained by simply acknowledging that whatever makes money is deemed “ethical.”
Sales Funnels
The sales funnel concept is crucial to understanding the modern medical industry. This method involves initially targeting a broad audience and then gradually narrowing down to more expensive products or services for the captured customers. There are typically two overlapping sales funnels in medicine:
The first funnel involves prescribing innocuous drugs to many people and then selling increasingly expensive pharmaceuticals to treat complications. For example, this often occurs with medications given to girls, leading to harmful consequences.
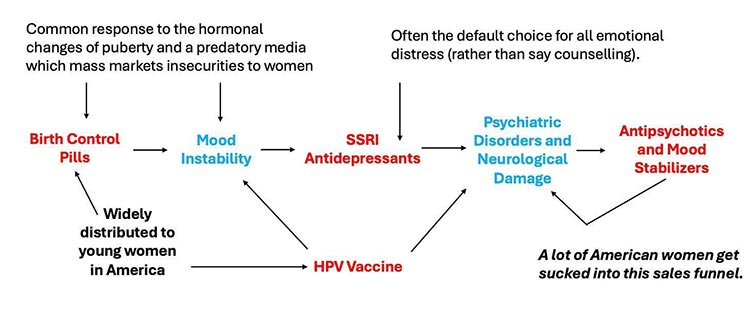
Note: Sources for the above graph can be found in this article about the dangers of SSRI antidepressants.1
The second funnel involves framing preventative medicine as screening individuals for potential health risks and then using these results to justify selling medical services like drug prescriptions. As these screenings become normalized, the industry expands the range of services offered, often leading to overdiagnosis and overtreatment. For instance, guidelines for “safe” blood pressure and cholesterol levels have been continuously lowered,2 hence putting more people on medications.
Note: The folly of this approach is highlighted by a trial that found removing on average 2.8 non-essential drugs from the elderly at one facility caused their 1-year death rate to go from 45% to 21%.3
DEXA Scams
One common way mass screenings are conducted is by giving many patients X-rays and then funneling those with abnormal imaging into being treated. For example, women over 50 get mammograms every two years to detect breast cancer early. However, studies show these screenings often lack overall benefit because fast-growing cancers are usually not caught early, while false positives are common and frequently lead to harmful treatments.
Note: Many medical specialists depend upon repeatedly performing the same billable service (e.g., vaccinating a child, performing a female pelvic exam, or reading a mammogram).
Another common universal screening practice for women is dual-energy X-ray absorptiometry (DEXA) scans, which measure bone density as an indicator of bone strength. The results are compared to the average bone density of a 30-year-old, producing a T-score. Medical students learn that a T-score of 0 to -1 is normal, -1 to -2.5 indicates osteopenia, and -2.5 or worse signifies osteoporosis, prompting urgent treatment.
However, considering natural age-related bone density loss, most individuals will have lower bone density than a 30-year-old. Thus, the current approach to managing osteoporosis acknowledges inevitable bone loss with age and focuses on prevention, as regaining bone density later in life is challenging.
How reliable are DEXA scans? Results vary significantly based on machine, operator, and measured bones, with studies showing a 5% – 6% difference4 in bone density. This variation can alter T-scores by 0.2 – 0.4, leading to misdiagnoses of osteoporosis.
Is repeated scanning necessary? A study of 4124 older women5 found no additional useful information gained from repeating DEXA scans over 8 years. Yet, guidelines recommend scans every 1-2 years, with Medicare covering one every 2 years, despite costs ranging from $150 to $300 per scan.
Do DEXA scans accurately predict fracture risk? While generally predictive, studies show discrepancies between scan results6 and observed bone strength under a microscope. Additionally, scans often underestimate strength loss in deliberately weakened bones.
Note: I recently learned from Dr. Mercola that a faster and more accurate method of diagnosing bone strength (which does not expose patients to ionizing radiation) is beginning to be used in Europe.7 REMS technology works by sending ultrasound waves8 into the bone and then analyzing the spectrum created to assess the health of the bones.
As this presentation shows, it accurately predicts bone density, and additionally, predicts bone strength. In short, this may be a dramatically superior approach to Dexa scans, but it faces stiff resistance in the United States because of how heavily invested many already are in performing Dexa scans. For those interested, more information can be found at EchoLight’s website.9

Note: This comment was affirmed in an NPR article.10

Save This Article for Later – Get the PDF Now
Bisphosphonates
Once osteoporosis is diagnosed, the initial treatment often involves starting a bisphosphonate, which may continue for 3-5 years depending on the administration method. A variety of factors influence the development of bone.
Two of the most important ones are the cells that build bone up (osteoblasts) and the cells that break bone down (osteoclasts). Bisphosphonates, (e.g., Fosamax or Actonel), concentrate in bones and inhibit osteoclasts,11 leading to increased bone density by shifting the balance towards bone building. However, this approach faces two major issues:
•Bisphosphonates are associated with numerous side effects,12 such as stomach irritation, severe muscle and bone pain, flu-like symptoms, osteonecrosis of the jaw,13 unusual hip fractures, atrial fibrillation, hypocalcemia, fatigue, and kidney problems. Remarkably, the American Dental Association even cautioned its members14 to avoid working on patients who are taking bisphosphonates.
•Bisphosphonates disrupt the body’s natural bone-building process, resulting in the preservation of “old bone” rather than promoting healthy bone formation.
Note: In addition to the bisphosphonates, there are other problematic osteoporosis drugs which also target the osteoclasts.
Bone Remodeling
One of the key adaptive processes in the body is its response to stresses and loads placed upon it. An often-overlooked marvel of the body is its continual reshaping of bones to bear loads optimally. While we seldom think about this process, its significance becomes apparent in certain scenarios. Consider space travel: astronauts, deprived of gravity’s weight signals, experience rapid bone loss,15 posing serious fracture risks upon returning to Earth.
In this bone-building ballet, osteoclasts play a crucial yet underappreciated role. They sculpt bones to withstand gravity’s demands, but when blocked by drugs like bisphosphonates, bones become denser yet more brittle and less flexible.
This underscores a common issue in medicine: focusing on treating numbers (e.g., lowering cholesterol) assuming it equates to health improvement. Studies often assess benefits through value changes (e.g., vaccine-induced antibodies), overlooking actual patient outcomes (e.g., in Pfizer’s COVID vaccine studies,16 antibody production didn’t correlate with decreased deaths).
In short, I would posit that while bisphosphonates may be effective at improving a DEXA score, they aren’t necessarily good at improving bone health.
What Causes Osteoporosis?
Bone metabolism is intricately linked to various key body processes, making it challenging to pinpoint the primary determinants of bone health. However, several factors stand out:
| Mobility — Sedentary lifestyles contribute to osteoporosis, highlighting the importance of weight-bearing activities in bone health.17 Walking is particularly beneficial and if done regularly throughout life dramatically improves bone health. |
| Hormones — In a previous article, I discussed the severe dangers of drugs like Lupron which work by disabling the body’s production of sex hormones. One of the most common side effects observed from them is a significant weakening of the bones. In turn, hormonal loss accompanying aging also weakens the bones. |
| Inflammation — Chronic inflammatory conditions increase the risk of osteoporosis by activating bone-dismantling processes.18 |
| Amino acids — Since one of the most essential components of bone health is the elasticity collagen imparts to them (as this allows bone to bend and yield to outside forces rather than shattering) collagen health is critically important for bone health.
In modern society, we are often deficient in those amino acids because of widespread stomach acid deficiency19 (which impairs our ability to metabolize protein into amino acids) and us predominantly consuming softer cuts of meat which lack the collagen building amino acids found in tougher parts of meat (e.g., gristle). Note: Colleagues such as Dr. Mercola have found consuming 30g – 40g of collagen each day sourced from beef knee joints is an optimal amino acid repletion protocol and in a short period of time significantly improves bone health (along with often improving a variety of related factors such as one’s height and one’s metabolic health). |
| Minerals — Dietary intake of minerals such as boron and manganese20 is crucial for bone strength, and deficiencies can impair bone health. Factors like stomach acid deficiency21 and soil depletion contribute to mineral deficiencies.
Note: The widespread deficiency of manganese in the population is in part due to it being chelated from the soil by glyphosate (Roundup).22 Manganese serves an essential role in building collagen, so when it is deficient, it frequently creates systemic ligamentous laxity,23 and in turn hypermobile patients such as those with EDS (who tend to be highly sensitive and susceptible to pharmaceutical injuries) notice a significant improvement in their ligamentous strength after a few months of appropriately dose manganese.24 |
| Water fluoridation — While fluoride increases bone density, it may compromise bone health and function. Some studies link fluoride to osteomalacia and increased fracture risk.25 |
| Pharmaceutical drugs — Medications like glucocorticoid steroids26 (e.g., prednisone) and opioids can weaken bones27 and increase fracture risk.
Note: Glucocorticoid induced bone loss is so severe it’s actually one of the few approved indications for bisphosphonate treatment.28 |
| Environmental toxins — Exposure to toxins like organophosphates, bisphenol A, nicotine, and heavy metals inhibits bone formation and contributes to osteoporosis.29 |
| Parathyroid adenomas — These tumors cause excessive secretion of parathyroid hormone, leading to calcium depletion from bones, bone loss, and a range of symptoms. Surprisingly, despite being a well-known condition, parathyroid adenomas are frequently missed. Identifying persistently elevated blood calcium levels can serve as a key indicator, prompting further investigation into a parathyroid adenomas. |
Note: Chinese Medicine has connected the age-related loss of the kidney’s vitality to bone loss for thousands of years. Many attribute this to the kidneys crucial role in regulating vitamin D and the blood levels of the minerals bone is composed of (e.g., calcium).
I suspect their regulation of the physiologic zeta potential (the decline of which is a key cause of aging) is also key. That is because zeta potential30 governs the tendency for blood to flow freely or clump together, and the hard exterior bone blood vessels must pass through makes them more susceptible to their blood supply becoming interrupted (e.g., from the bone moving out of place).
Conclusion
It’s fascinating to realize that bone is far more than just a structural component; it’s a living tissue with its own dynamic behavior. When I’ve had the opportunity to handle bone directly, such as during orthopedic surgeries, it’s evident how different it is from the lifeless bones we typically encounter. Unfortunately, this experience is rare, leading many to see bone as inert and unchanging.
The points I’ve discussed in this article are founded on the importance of recognizing bone’s vitality and understanding how our interactions with it shape our health and longevity. Ancient medical traditions, like Chinese medicine, appreciated this aspect of bone health. They saw it as integral to overall well-being, acknowledging its interconnectedness with the body’s systems.
By embracing this perspective, we can gain new insights into bone health and its significance for holistic healthcare. It’s my hope that this article sheds light on the dynamic nature of bones and encourages a deeper understanding of their role in our health journey.
Author’s note: This is an abridged version of a longer article on the subject which discusses the above points in more detail and many others such as our other preferred approaches for improving bone health. That article and its additional references can be read here.
A Note From Dr. Mercola About the Author
A Midwestern Doctor (AMD) is a board-certified physician in the Midwest and a longtime reader of Mercola.com. I appreciate his exceptional insight on a wide range of topics and I’m grateful to share them. I also respect his desire to remain anonymous as he is still on the front lines treating patients. To find more of AMD’s work, be sure to check out The Forgotten Side of Medicine on Substack.
- 1 Why Are Antidepressants So Harmful? November 27, 2023
- 2 What Can Statins Teach Us About The COVID-19 Vaccines? May 4, 2023
- 3 Israel Medical Association Journal 2007 June; 9(6):430-4
- 4 Medpage Today November 3, 2014
- 5 JAMA January 22, 2007
- 6 Indian Journal of Orthopedics Jan-Mar 2010; 44(1): 73–78
- 7, 9 ECHOLIGHT Medical, Accessed April 2024
- 8 Diagnostics (Basel). May 2023; 13(10): 1666
- 10 NPR, December 21, 2009
- 11 Mayo Clin Proc. September 2008; 83(9): 1032–1045
- 12 BMJ January 2008 19; 336(7636): 117
- 13 BMJ August 8, 2009
- 14 American Dental Association Accessed February 2008 (Archived)
- 15 International Journal of Molecular Sciences May 2021; 22(9): 4585
- 16 New England Journal of Medicine 2021;385:1761-73
- 17 Gynecological Endocrinology September 2009;25(9):616-20
- 18 Journal of Musculoskeletal and Neuronal Interactions 2020; 20(3): 372–381
- 19, 21 Stomach Acid Is Good For You, September 16, 2023
- 20, 23, 24 The Hidden Link Between Hypermobility and Vaccine Injury, January 14, 2024
- 22 Surgical Neurology International. 2015; 6: 45
- 25 Fluoride Action Network April 2012
- 26 RMD Open. 2015; 1(1): e000014
- 27 Addiction, July 2019
- 28 FDA, 2012
- 29 OuluREPO, 2016
- 30 What Makes All Vaccines So Dangerous? March 31, 2024














Thanks! Share it with your friends!
Tweet
Share
Pin It
LinkedIn
Google+
Reddit
Tumblr