STORY AT-A-GLANCE
- Gut health plays a crucial role in nutrient absorption, hormone balance, energy levels, mood, and inflammation
- A healthy gut typically involves regular bowel movements (1-3 times a day), minimal skin issues, and the ability to enjoy a variety of foods without discomfort
- Your gut lining regenerates every three days, and your gut microbiome can change daily based on diet, suggesting that lengthy gut healing protocols are unnecessary
- Hypothyroidism can reduce stomach acid and other digestive juices, leading to bloating, constipation, and food allergies due to its effect on gut motility and enzyme production
- Maintaining a good energetic state is crucial for gut health, as systemic energy production influences digestive processes and microbial balance in the gut
Gut health is incredibly important for our overall health and the state of our gut plays a huge role in how we respond to foods and the environment, how we absorb nutrients, hormone health, our energy and mood, systemic inflammation, and so much more.
But instead of finding the root cause of gut issues, symptoms are commonly addressed with band-aid treatments.
If you have heartburn, you are prescribed an antacid (which further lowers your stomach acid levels). If you have IBS this is treated with fiber, laxatives and sometimes an antidepressant. If you have food sensitivities, you are told to remove this food … but none of these Band-Aids fix the root cause of the issue.
We have to understand why the gut got to where it is right now — what lifestyle and dietary choices led us to the current state.
But What Even Is Good Gut Health?
Given that we are all in different environments, have different pasts, eat different foods, and have different day to day activities — there is no one single way to define a ‘good’ gut health. But in general, with a properly functioning digestive system you should have …
- Daily poops (at least 1 time a day, ideally 2-3), solid structure, easy to pass. The more we can poop, the better we will feel! You should be pooping at least 1X a day.
- Minimal skin or acne issues.
- Relief from bloating or stomach discomfort after meals.
- Enjoy a wide range of food, within reason, without experiencing severe issues. You shouldn’t have to extremely restrict your food in the long run. Having a lot of food intolerances is a sign of a sluggish digestive system.
Just like every system in the body, digestion is energy dependent.
“Systemic metabolic problems make local problems worse” ~ Dr. Ray Peat
Thyroid health and energy metabolism are intimately involved since the thyroid is the metabolic regulator. In hypothyroidism there is less stomach acid and other digestive juices, so gas, slow transit time, food allergies, bloating and constipation are common.
But the good news: The lining of the gut is replaced every THREE DAYS!1 And on top of that, your gut microbiome can change within a single day based on what you eat.2
Meaning, long gut healing protocols don’t make ANY sense. This doesn’t mean you will fix your gut overnight — just sharing to motivate and encourage you that your gut can and will heal. It won’t take 1 day, but it also shouldn’t take years.
If you are still trying to fix your gut several months or years later, the approach you are taking may not be working.
How Do You Fix Gut Health?
For most individuals, I believe in a rather stand-offish approach for the gut as I believe that we should not interfere with Mother Nature. The microbiome is incredibly complex, and rather than trying to micro manipulate, I truly believe in giving her the tools and resources, and letting her do her thing.
Pooping 1-3 times a day, and giving the digestive system adequate energy and nutrients — and she will fix herself. But you have to be in a good energetic state for this to happen. There are now thousands of studies in the literature documenting the connection between digestive health and thyroid health.3
And while many of these studies are for ‘clinical’ hypothyroidism, subclinical hypothyroidism will still manifest as some sort of digestive issue, maybe not as severe, since any down regulation in systemic energy production will negatively impact digestion, a very energy intensive process.
Let’s analyze examples of how energy production and thyroid health are intimately connected to gut health:
•Gut lining health — The length and thickness of the intestinal villi, which determines the thickness, permeability and strength of the intestinal lining, is impacted by thyroid health. “In hypothyroidism, the intestinal villi were short and the intestinal wall (muscle layer) was thickened, thereby increasing intestinal tone and leading to reduced intestinal motility.”4,5
Active thyroid hormone (T3) is a critical regulator of intestinal epithelial and gut mucosal development, differentiation and homeostasis.6,7
•Gut motility — Hypothyroidism leads to slower gastric emptying times.8,9,10
?In one study comparing hypothyroid patients to a healthy patient:11
?Esophageal emptying
?Healthy patient = 90.13%
?Hypothyroid patient = 57.83%
?Esophageal transit time
?Healthy patient = 21.5 sec
?Hypothyroid patient = 50.5 sec
?Gastric emptying half-time
?Healthy patient = 28.43 min
?Hypothyroid patient = 79.48 min
?“Hypothyroidism affects the entire gastrointestinal system and causes hypomotility.”
Thyroid hormones are known to influence gut motility by modulating the ENS and altering smooth muscle function and the MMC12,13 essentially down regulating the motor activity of the digestive system.
Slowed motility can quickly lead to digestive issues as the slower your digestion, the more food your bacteria gets, so the more time bacteria has to ferment that food.
•Digestive enzymes and bile
?Low T3 (active thyroid hormone) leads to poor stomach acid secretion.14
?Moreover, thyroid health is intricately connected to liver health and thus the amount of bile your body produces and releases.15
•Dysbiosis
?Thyroid status is linked to the composition of the gut.16 Meaning, the health of ones thyroid system will impact the microbiome balance.
?Dysbiosis is common in those with thyroid disorders.17
Your energetic state impacts your internal environment, and your internal environment impacts how your body (and gut) functions. The composition of the gut microbiome is extremely complex.
And while it is near impossible to define what the ideal microbiome should look like (resident microbes are highly diverse, vary between individuals, and change with diet), recent evidence supports that colonic bacteria should be dominated by obligate anaerobic bacteria that are able to benefit us by breaking down non-usable fibers with lower levels of facultative organisms since these facultative anaerobic bacteria do not specialize in consuming fiber and might even interfere with host nutrition.18 (Plus, they produce really problematic endotoxins that wreak havoc in the body!)
Now, we will always have some amount of both obligate and facultative species, but balanced gut microbiomes are characterized by the dominance of obligate organisms, while an expansion of facultative organisms is a common marker of gut dysbiosis.
We want more obligate anaerobic bacteria, but these beneficial species cannot survive in high oxygen environments. (While facultative anaerobes, on the other hand, grow well in the presence of oxygen.)
So maintaining a LOW oxygen environment and thus a HIGH CO2 environment in our gut helps keep the microbiome in check. And you cannot maintain a high CO2 level without a high metabolic rate and good energy production. (Which can be assessed by body temperature measurements.)
The metabolism of the cells that line your gut, meaning how they make energy, changes the internal environment of the gut, thus impacting the types of bacteria that can thrive.
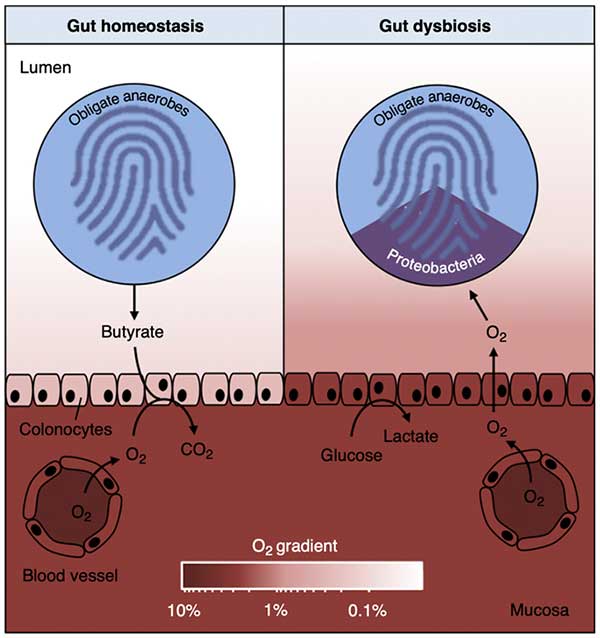
“During gut homeostasis (left), b-oxidation of microbiota-derived butyrate causes epithelial hypoxia, which maintains anaerobiasis in the lumen of the large bowel. In turn, luminal anaerobiasis drives a dominance of obligate anaerobic bacteria within the gut microbiota. During gut dysbiosis (right), surface colonocytes obtain energy by anaerobic glycolysis, which leads to increased epithelial oxygenation. This epithelial dysfunction disrupts anaerobiasis in the lumen, thereby driving an expansion of facultative anaerobic Proteobacteria by aerobic respiration. The color scale shown at the bottom (O2 gradient) indicates oxygen availability.” Image from COMICR Volume 39, October 2017, Pages 1-6.
These cells have two options for energy production: beta oxidation or glycolysis. Ideally, they perform oxidative phosphorylation through beta oxidation of short chain fatty acids (SCFAs) — that can come from the food we eat like butter, or from obligate anaerobes (the types of bacteria we want in our gut that can only survive in low oxygen environments) breaking down fiber, or both.
Butyrate oxidation consumes high amounts of oxygen, which then maintains a low oxygen environment inside the colon.
Glycolysis, on the other hand, is relied on more when someone is in a LOW ENERGY state. Glycolysis doesn’t use up nearly as much oxygen, thus leading to a high oxygen state inside the gut. This type of high oxygen environment allows facultative anaerobes and pathogens to take over.
Inflammatory signals and low levels of systemic energy production can shift the colonocyte metabolism towards anaerobic glycolysis19 thereby lowering oxygen consumption and lowering ATP generation, which ultimately leads to a shift in the microbial community from obligate to facultative anaerobic bacteria due to a higher oxygen environment.20,21 Enter dysbiosis.
“The energy metabolism of colonic epithelial cells functions as a control switch of the gut microbiota, mediating shifts between homeostatic and dysbiotic communities.”
The left side of the image is what we want to happen, where there is a low oxygen environment. The epithelial cells perform beta oxidation which uses up a lot of oxygen and produces a lot of ATP. On the right, the gut lining cells instead perform glycolysis, less oxygen is used so the inside of the gut has higher oxygen levels, and creates an ideal environment for facultative bacteria to thrive, inducing dysbiosis.
Plus, excessive glycolysis means less energy is produced, so the gut lining cells will have less energy to maintain structure and function.
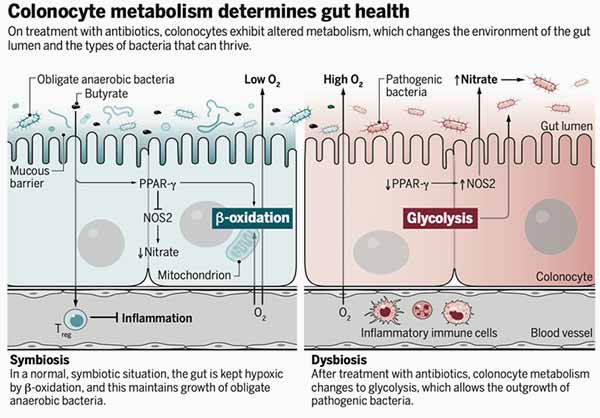
A low oxygen environment inside the colon ensures the colonic microbiota is dominated by obligate anaerobic bacteria, which provide benefits to us by converting fiber and food waste into short chain fatty acids, the food source for our gut lining cells. Higher oxygen levels inside the colon increases the population of facultative anaerobic bacteria. Image from SCIENCE Volume 357, 11 Aug 2017, Issue 6351.
So instead of trying to micro manipulate the microbiome, the body can find the right balance of microbes when given the right environment and sufficient energy. Even if you temporarily ‘fix’ your gut with a supplement or short-term restriction — if you don’t fix the underlying low energetic state that led to the high oxygen gut state to begin with — there is a high chance you will end up back to where you started.
I share all of this to again remind you that fixing how the body produces energy at the systemic level will improve gut health. Understanding systemic energy production is also FREEING — as there is nothing wrong with you! You are just slightly out of balance.
Every part of the digestive process requires cellular energy, so every part of digestive function can be impacted with low energy production.
So, subclinical or clinical hypothyroidism, and thus hindered energy production, is one of, if not the root cause of most digestive issues. And you don’t have to go to extremes to fix your gut health (in fact, extremes can often lead to long-term gut health problems).
Instead, the focus should always be on improving metabolic rate and systemic function. When the body is working as intended, gut health will improve!

Save This Article for Later – Get the PDF Now
Transform Your Health — One Step at a Time

Ashley and her sister Sarah have put together a truly groundbreaking step-by-step course called “Rooted in Resilience.” They have compiled what clearly is the best application of Dr. Ray Peat’s work on Bioenergetic Medicine that I have ever seen.
It is so good that I am using the core of their program to teach the many Health Coaches that I am in the process of training for the new Mercola Health Clinics I am opening this fall. It took these women working nearly full-time on this project for a year to create it.
This has to be one of the absolute best values for health education I have ever seen. If you want to understand why you struggle with health problems and then have a clear program on how to reverse those challenges, then this is the course for you.
It is precisely the type of program I wish I would have had access to when I got out of medical school. I fumbled around for decades before I reached the conclusion they discuss in the course and share with you so you can restore your cellular energy production and recover your health.
| Select and eat the right foods to heal your metabolism and improve glucose utilization |
| Balance your hormones to help reduce anxiety, weight gain and sleep disturbances |
| Use reverse dieting to increase your calories without gaining weight and tanking your metabolism, all while improving your energy levels |
| Heal your gut for proper immune function, mood and weight management |
| Tweak your diet and lifestyle habits to improve your mindset and mental health |
| Crush your fitness goals with ease and get your life back on track |
| Master the most essential habits for health with bonus guides, including over 100 meal plans to take the stress out of meal time planning and shopping, and so much more! |
Learn more about Rooted in Resilience here.

About the Author
Ashley Armstrong is the cofounder of Angel Acres Egg Co., which specializes in low-PUFA (polyunsaturated fat) eggs that are shipped to all 50 states (join waitlist here), and Nourish Cooperative, which ships low-PUFA pork, beef, cheese, A2 dairy and traditional sourdough to all 50 states. Waitlists will reopen shortly.
- 1 Frontiers in Cell and Developmental Biology 12 November 2020 Sec. Stem Cell Research
- 2 Science Translational Medicine 2009 Nov 11;1(6):6ra14
- 3 World Journal Gastroenterol 2009 Jun 21; 15(23): 2834–2838
- 4 Nigerian Journal of Physiological Science 2015 Dec 20;30(1-2):59-64
- 5 The Journal of Endocrinology 1996 Dec;151(3):431-7
- 6 Molecular Endocrinology 2004 Aug;18(8):1941-62
- 7 Journal of Gastrointestinal Surgery 2001 Jan-Feb;5(1):49-55
- 8 Indian Journal Endocrinology Metab. 2014 May-Jun; 18(3): 307–309
- 9, 11 Gastroenterology Research and Practice 2009; 2009: 529802
- 10 Israel Journal of Medical Sciences 1997 Mar;33(3):198-203
- 12 Neuropeptides 1996 Jun;30(3):237-47
- 13 Handbook of Clinical Neurology 86:343-55 DOI: 10.1016/S0072-9752(07)86017-9
- 14 Acta Endocrinologica (Copenh) 1980 Nov;95(3):341-9. doi: 10.1530/acta.0.0950341
- 15 QJM: An International Journal of Medicine, Volume 95, Issue 9, September 2002
- 16 Trends in Endocrinology and Metabolism 2019 Aug;30(8):479-490. doi: 10.1016/j.tem.2019.05.008
- 17 Nutrients 2020 Jun; 12(6): 1769
- 18, 20 Science 2018 Nov 30; 362(6418): eaat9076. doi: 10.1126/science.aat9076
- 19 Cell Host Microbe 2018 Jan 10;23(1):54-64.e6. doi: 10.1016/j.chom.2017.11.006. Epub 2017 Dec 21
- 21 Science 2017 Aug 11; 357(6351): 570–575. doi: 10.1126/science.aam9949



















Thanks! Share it with your friends!
Tweet
Share
Pin It
LinkedIn
Google+
Reddit
Tumblr