STORY AT-A-GLANCE
- Health authorities and the World Economic Forum predict that millions of people will be dying from superbugs every year by 2050
- According to the WEF, antimicrobial resistance is a “looming health catastrophe that could be more deadly than COVID-19”
- They are calling for a new “subscription model” as a solution and a “political intervention to reconstruct the market and make the development, production of and marketing antibiotics profitable again”
- While there is no reason to believe the WEF on anything, antimicrobial resistance is on the rise due to overuse of antibiotics in medicine and agriculture, antibiotics into water supply, overuse of antibacterial household products, and weakened immunity due to stress and toxins
- Superbug infections are particularly alarming in hospital settings
This story is about antimicrobial resistance, a real and potentially serious medical issue, as well as a new scarecrow and cash cow of the pharmaceutical and biochemical industries and their investors.
Let’s Start With the Foundations
Human body is mysterious and amazing, made with wisdom and care. It is simply amazing how well we are designed to deal with natural dangers, and how many healing foods and medicines nature has for us when we need a lift in our defenses. As a species, all we have to do is to be humble, curious, balanced, and grateful, and to live in harmony with nature as opposed to try to fight it. So much love and beauty!
Sadly, there is an ongoing attack on our ability to live in harmony with nature. As it often goes, we tend to not think about those things early on due to constant brainwashing and manufactured distractions — but sooner or later, the laws of nature catch up to us, and many develop health issues — and then start on a journey of rediscovering the basic things about health and life.
Many people are forced to figure it out the hard way due to developing a chronic disease. Others, otherwise healthy, are very sensitive to environmental toxins, and their bodies react to pollution dramatically and immediately (and of course, those two conditions are often interrelated).
In a way, we, the modern people at the mercy of the Rockefeller food and medicine, are like innocent puppies in a lab. Our handlers feed us poisons in food, water, air, clothes, furniture, homes, drugs, and vaccines — and we take them because by default, we don’t expect such “surround” treachery.
But sooner or later, we start noticing problems, and we learn, and the abuse becomes apparent to our eyes. And once we learn, we try to warn others who are still oblivious to the poisoning process — and then they think we are crazy because they are still not at a point where they feel it or make the connection.
In a sense, living in today’s world is extremely confusing and abusive — but we don’t think about it as kids because this broken world of ours is the only world we know, it’s the world of our parents and grandparents, it’s the default — and we only start to think about it when our bodies react to abuse in a visible way.
We, the people of today, are born into a giant abusive experiment made from scraps of incredible beauty. And yes, we pay the price for the imbalance. But as we pay the price, as we walk the journey and rediscover the basics, as we cry and scream and wonder why we’ve duped so badly — we remember our souls at last, and then there is no stopping us. Once we remember our souls, there is no stopping us. There is no stopping us.
The World Economic Forum on Antimicrobial Resistance
What do our “masters” have to say about antimicrobial resistance? The World Economic Forum, for example, has a lot to say! They have pages and pages of search results on the topic.
According to this WEF article, tellingly titled, “This is how to fight antibiotic-resistant superbugs with a simple subscription payment model,” people are now dying from infections that had been previously treatable.
There’s not a peep by the WEF about the fact that superbugs are a prime demonstration of what happens when people get arrogant and start fighting nature without understanding all the intricate connections, while pursuing mainly profit. There’s not a peep about how the Rockefeller medicine model is outright toxic.
The WEF’s “solution” to the problem of antimicrobial resistance is of course to love pharma companies a little more, give them more money in a guaranteed manner, and that’ll solve it. In other words, it’s the “new normal” for us peasant — and business as usual for pharma, with more sass.
What I find alarming is that various WEF articles about antimicrobial resistance talk about how currently, there is “no market” for new antibiotics, and it’s a problem, and so we need to develop a market, and drum up the funding (taxpayer money, without a doubt), etc. etc.
It makes me think about that one time when Peter Daszak lamented that there was no perceived need for pan-influenza and pan-coronavirus vaccines — and then we got COVID! A quote from the WEF article:
“The solution requires political intervention to reconstruct the market and make the development, production of and marketing antibiotics profitable again. We need to change the way we value antibiotics — by paying for reliable and sustainable access to these lifesaving drugs.”
Notably, they say that millions of people may be dying from superbugs every year by 2050. That prediction is based on models. So just to be clear, they are touting this “prediction,” but they also have a lot of public and industry figures captured, and their predictions are a bit like business goals that are worked on by an impressive staff, consisting of world and industry leaders.
In that light, I find the prediction alarming, especially given that certain safe and effective medical products seem to mess with people’s immune systems, and that there is a war on natural immunity altogether.
Plus, antimicrobial resistance is genuinely on the rise, and people innate immunity is on the overall decline due to a wide range of poisons, as well as lockdowns and other “health” measures, including mad spaying of antibacterial products on everything, to save us all from COVID. The use of antibacterial products and sanitizers from here to horizon can’t be good for us in the context of antimicrobial resistance, can it?
And here’s more from the WEF article called, “The looming health catastrophe that could be more deadly than COVID-19”:
“Superbugs. You’ve probably heard of them, but did you know they’re one of the biggest threats to global public health? Left unchecked, these drug-resistant bugs could kill millions of people every year with the damage to health potentially dwarfing that of COVID-19, according to the AMR action fund.”
“That makes antimicrobial resistance, or AMR, a top 10 global public health threat, according to the World Health Organization, which is raising awareness and promoting ways forward with World Antimicrobial Awareness Week.”
“Tackling resistance matters because the problem has the potential to spiral, with the AMR Action Fund estimating that deaths from antibiotic-resistant infections could rise to around 10 million a year by 2050, up from around 700,000 in 2019. And it could cost the global economy as much as $100 trillion between now and 2050.”
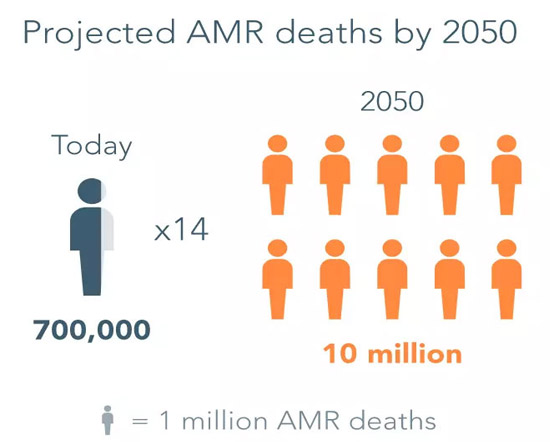 Image: AMR Action Fund
Image: AMR Action FundAnd here is a quote that reveals their thinking. And while in general, it makes sense that R&D requires funding, the comment about no current market makes it a little alarming, in the light of the general trends.
“‘There is currently no viable market for the development of new antibiotics,’ says Kasim Kutay, CEO of Novo Holdings, which administers the investment in the AMR Action Fund on behalf of the Novo Nordisk Foundation. ‘As a result, antibiotics that are in the early stages of development never reach patients because of a lack of funding for the later stages of clinical research. The AMR Action Fund is an important part of the solution to this.'”
And here is another WEF article from 2021, titled “Optimism despite COVID-19 impact on antimicrobial resistance”:
“The pipeline of new antibiotics is running dry, because the market for antibiotics is broken. The development costs for newly approved antibiotics cannot be covered through sales. Most of the major pharmaceutical companies have stopped developing new antibiotics, and many smaller enterprises have folded due to the lack of a sustainable economic model.
The main reason is that newly developed, effective antibiotics are being used as a ‘last resort’ in the hospital sector: they are sensibly kept locked away in the medical cabinet, only to be used if the cheap generics fail. Of course, this is damaging to the manufacturers’ incentive, as it undermines the possibility to make revenues from new antibiotics. [emphasis mine]“
They even a paraphrase of the same “call for action” for the politicians. So it seems like the World Economic Forum people are really drumming their fingers, demanding a political interference into the market (do we have a free market?):
“The solution requires political intervention to reconstruct the market and make the development and production of antibiotics profitable again. We need to change the way we value antibiotics to make-up for costly development.”
Me, a peasant at heart, is thinking, maybe there is no market because people aren’t that scared? And maybe, the real danger for the “market” is that the Rockefeller medicine model is visibly failing on so many fronts, and the orchestrated destructive “COVID response” has opened many eyes, and now the “masters” are worried that people will turn to “alternative” treatments that could potentially treat the bugs that have developed a residence to pharmaceutical products — and stop contributing the pharma industry pockets?
So they want to scare us senseless to ensure that we refrain from acting in our best interests and continue being enchanted? Maybe that’s what’s happening?
And by the way, I think that there can be different ways to treat a disease, and it’s good to be open-minded and generally use common sense and discretion. And modern medicine can be life-saving when used in balance, even though our ancestors probably didn’t need many of the treatments that we use today because they were exposed to more nature and less pollution, and weren’t being constantly poisoned.
There are medicines for different times and different circumstances and different people — but what is certain is that our medical system at large is very broken, and there is no reason to trust it blindly. I am being very diplomatic with this statement.
Asymptomatic Transmission of Superbugs?
Another trend that I find potentially alarming in the aftermath of the COVID “health response” and the conversation about the asymptomatic transmission of superbugs.
Even if it may be wise to keep in mind the possibility of asymptomatic carrying and potential transmission of some bacterial or fungal infections — and we do carry a lot of bugs at all times, and can typically handle them just fine, unless our body is broken or poisoned — if the “COVID testing principle” is applied, then all citizens might be asked to perpetually test for everything “so as not to kill the grandma.,” etc. And that would be ugly. Profitable to the masters but ugly.
Plus, quite a few of those superbug infections come from the hospital settings and medical devices — so using more devices to protect us from superbugs is hardly a useful solution. Here’s from Healthline:
“For some people, being infected with a superbug causes no symptoms at all. When healthy people carry germs without being symptomatic, they can infect vulnerable people without even realizing it.”
Like I said, it really depends on where they take this. More from Healthline:
“According to the 2019 Antibiotic Resistance Threat Report, published by the Centers for Disease Control and Prevention (CDC), more than 2.8 million drug-resistant infections happen every year in the United States, and more than 35,000 of them are fatal.”
“The CDC’s report lists 18 bacteria and fungi that endanger human health, classifying them as either: urgent, serious, concerning threats.”
Urgent threats
- Carbapenem-resistant Acinetobacter
- Candida auris
- Clostridioides difficile
- Carbapenem-resistant Enterobacteriaceae
- Drug-resistant Neisseria gonorrhoeae
Serious threats
- Drug-resistant Campylobacter
- Drug-resistant Candida
- ESBL-producing Enterobacteriaceae
- Vancomycin-resistant Enterococci (VRE)
- Multidrug-resistant Pseudomonas aeruginosa
- Drug-resistant nontyphoidal Salmonella
- Drug-resistant Salmonella serotype Typhi
- Drug-resistant Shigella
- Methicillin-resistant Staphylococcus aureus (MRSA)
- Drug-resistant Streptococcus pneumoniae
- Drug-resistant Tuberculosis
Concerning threats
- Erythromycin-resistant group A Streptococcus
- Clindamycin-resistant group B Streptococcus
What Does the Most Trustworthy Health Authority in the World, the World Health Organization, Have to Say About Antimicrobial Resistance?
The World Health Organization (or their social media person) wants us to “unite to preserve antimicrobials,” which kind of gives away the focus of the WHO on the pharmaceutical industry as opposed to people:
Here is another tweet by the WHO in which they instruct the people on how to fight against the danger of AMR (never mind the extensive use of antibiotics in agriculture and all sorts of chemical pollution that messes with our immunity).
Interestingly, the list includes “preventing infections.” I don’t know, after all we’ve been through, a call to “prevent infections” makes me nervous. Are they developing new experimental medical products to shove down our throats, or will they ask us all to wear butt plugs to prevent potentially infectious … I am not going to say it? It’s 2022, nothing is off the table!
And here’s the WHO on One Health Global Leaders Group on Antimicrobial Resistance (I guess, there are so many words in the English language, and it’s hard to avoid the phrase “global leaders”):
The Directors General described the rapid rise of antimicrobial resistance as one of the world’s most urgent threats to human, animal, plant and environmental health – endangering food security, international trade, economic development and undermining progress towards the Sustainable Development Goals (SDGs).
Pasteur Act in the U.S.
In June 2021, Pasteur Act was introduced into Senate, and it does exactly what the World Economic Forum has been drumming its fingers about:
“This bill authorizes the Department of Health and Human Services (HHS) to enter into subscription contracts for critical-need antimicrobial drugs, provides $11 billion in appropriations for activities under the bill, and contains other related provisions.”
It seems like according to the bill, the definition of an “antimicrobial drug” does not include “vaccines” (although the new official definition of vaccines is so broad that it includes therapeutics, so honestly we don’t know at this point).
WEF on the Pasteur Act and the Recent Developments in AMR
The WEB lists the following developments on the AMR front:
- Introduction in the US of the PASTEUR Act, which aims to kick-start the development of urgently needed new antibiotics by changing the way the US government pays for them.
- Progress on Swedish and UK government models implementing new AMR payment structures targeted at rebooting the broken marketplace.
- The EU is to address several AMR challenges, including the lack of investment in antimicrobials and inappropriate use of antibiotics, as appears from the recent Pharmaceutical Strategy for Europe adopted by the Commission in November 2020.
- The AMR Action Fund has raised US$1 billion from major pharmaceutical companies and foundations to invest in biotech. The aim is to bring as many as four new antibiotics to patients by 2030.
Resistant Candida Species
Fungi, and in particular Candida species, are among the resistant bugs that are on the rise. As a side note, a lot of the symptoms of systemic Candida infection overlap with the symptoms of “long COVID,” and this is food for thought. Here is the CDC on resistant Candida species.
“Antifungal resistance is an increasing problem with the fungus Candida, a yeast. Candida infections may resist antifungal drugs, making them difficult to treat.
About 7% of all Candida blood samples tested at CDC are resistant to the antifungal drug fluconazole. Although one Candida species, Candida albicans, is the most common cause of severe Candida infections, resistance is most common in other species, particularly Candida auris, Candida glabrata, and Candida parapsilosis.1
Concern is rising over the emerging fungus Candida auris,2 which is rare in most areas of the United States but is a growing threat. Resistance rates for C. auris are much higher than for other Candida species, with:
- About 90% of U.S. C. auris samples being resistant to fluconazole, and
- Up to one-third are resistant to the antifungal drug amphotericin B”
By the way, here is a Newsweek article titled, “Drug-Resistant Candida auris Fungus Found in Louisiana for First Time, Weeks After Oregon”:
“Candida auris is an emerging fungus in the U.S., with cases mostly occurring after mid-2015, according to the Council of State and Territorial Epidemiologists in 2018. It has been reported from over 30 countries overall … Candida auris presents a serious global health threat with most cases of infection resulting from local spread within health care facilities. There have been over 1,150 clinical cases in the U.S. since 2013.”
“In some patients it can cause severe illness and death, entering the bloodstream and spreading throughout the body. Patients who have been hospitalized for a long time, have lines or tubes entering the body, or who have previously received antibiotics or antifungal medicines appear to be at highest risk of infection.”
“The CDC states that based on information from a limited number of patients, 30 to 60 percent of people infected with the fungus have died. However, many of these patients have had other serious illnesses as well.”
“Part of the concern surrounding Candida auris is that it is resistant to multiple antifungal drugs. Some strains are resistant to all three available classes of antifungals, the CDC states, making infection with these strains even more difficult to treat.”
Nature to the Rescue
Interestingly, there is a number of studies showing the effectiveness of various plants and natural antifungals against various species of Candida. Since I am an artist and a journalist, not a doctor, and since I don’t want to get anything accidentally banned once the censors sense a new danger to the profits of their masters, I am just going to point to this study, published at the NIH website, titled, “Plants’ Natural Products as Alternative Promising Anti-Candida Drugs.”
All in all, I think that given where the wind is blowing, now is a very good time to learn about natural antifungals, as well is to really invest into boosting (sorry not that kind of boosting) our immunity and developing good habits that support a healthy microbiome, since a healthy microbiome is very important for our health, including the immune system.
I think we might be heading toward a tsunami of toxicity-driven health issues that are related to a disrupted microbial balance, and we better be in our best shape as much as we can, and in high spirits as well.
Microbiome and COVID
It is amazing how complex the human body is, and how little the scientists really know about it. The importance of maintaining a wholesome microbiome is rarely (if at all) talked about in the mainstream but it turns out that there is a direct correlation between the diversity of the gut microbiome and even the severity of COVID symptoms!
For example, this study by Dr. Sabine Hazan et al. is an eye-opener. According to the study, severely symptomatic patients had “less bacterial diversity,” and “positive patients overall had lower relative abundances of Bifidobacterium, Faecalibacterium, and Roseburium, while having increased Bacteroides.” There was an “inverse association between disease severity and abundance of the same bacteria.”
On the positive role of Bifidobacteria, here is another study by Dr. Sabine, titled, “Pre-Existing Microbiome Signature in a SARS-CoV-2 Discordant Family,” in which she looks at the differences in gut microbiomes of the index patient and his mother. (And yes, the question of the intrinsic reliability of the PCR test is another matter, but the study is very interesting.)
“Our index patient is a 19-year-old man with Crohn’s disease. After developing symptoms consistent with COVID-19, he, his 62-year-old father, and 14-year-old sister tested positive for SARS-CoV-2 in May 2020. Despite a shared household, his 50-year-old mother with a history of asthma and his healthy brother and sister-in-law (a married couple) remained negative.
The index patient and his mother had undergone microbiome analysis in May 2019, following his brother and his sister-in-law in November 2020. We observed significant differences between the fecal microbiota of the SARS-CoV-2-positive son and those of his healthy family.
There were differences in the bacterial phylum, class, order, family, and genus level with the increased relative abundance of Bacteroidetes and reductions or deletions in bacterial diversity, particularly of the Bifidobacterium family. This unique study may signal a new exploratory avenue for the prevention or treatment of SARS-CoV-2 infections.”
Notably, it’s been shown that probiotics tend to improve long COVD.
Microbiome and Parasites
Here is an interesting preliminary observation regarding the tight relationship between gut microbiome and parasite infections. The authors don’t claim to know whether the difference in microbiome determined the susceptibility to parasite infection or whether it could be attributed to the parasite infection itself. But the research is definitely interesting.
“In Genome Biology, a study led by University of Pennsylvania scientists investigated the links between parasite infection and the gut microbiome.
Using genetic methods to characterize the gastrointestinal microbiome of 575 ethnically diverse Cameroonian people representing populations from nine villages with meaningful differences in lifestyle, the researchers discovered that the presence of parasites was strongly associated with the overall composition of the microbiome.”
Conclusion
In conclusion, I would like to say that we are in a phase of history where the limitations and the “side effects” of the algorithmic, pharma-driven model of medicine are getting obvious to more people, and that is the reason for all the bullying. What I think will happen is that a lot of people will flee the toxic, trap-setting Rockefeller medicine, and no threats and no temptation will be able to stop the exodus.
May we re-discover the joy of living in good health, the joy of being in harmony with our soul and with nature. We know what’s good for us, and there is no stopping us.
About the Author
To find more of Tessa Lena’s work, be sure to check out her bio, Tessa Fights Robots.

















Thanks! Share it with your friends!
Tweet
Share
Pin It
LinkedIn
Google+
Reddit
Tumblr